Dr John Kariuki could have been one of the 1.27 million people who died from Antimicrobial Resistance (AMR) in 2019.
Dr Kariuki, a veterinarian, acquired an infection from the hospital, and his life changed for good.
"I was very close to death, and when I eventually managed to treat it, it was almost too late, I am now living with a disability thanks to AMR," he narrates.
He says that instead of spending 5000 USD, "I ended up spending 35,000 USD. This is something that could have been avoided if prevention measures were taken in good time."
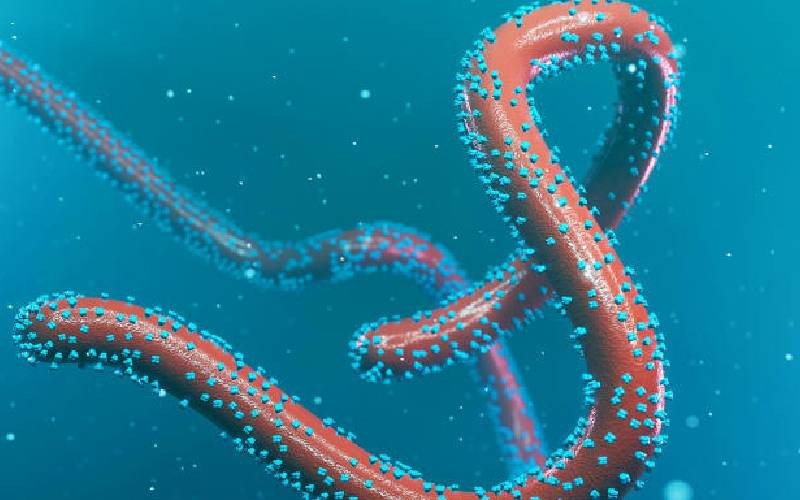
According to the World Health Organisation (WHO), AMR occurs when bacteria, viruses, fungi, and parasites no longer respond to antimicrobial agents. As a result of drug resistance, antibiotics, and other antimicrobial agents become ineffective, and infections become difficult or impossible to treat, increasing the risk of disease spread, severe illness, and death.
World Antimicrobial Awareness Week (WAAW) is marked annually from November 18 to 24. During this period, the Ministries of Health, Environment, Climate Change and Forestry, Mining, Blue Economy and Maritime Affairs, and Livestock and Agriculture, together with other stakeholders, have collaborated to work around the theme for this year: "Educate, Advocate, Act Now."
- Hydration hacks: When, and how much water should you really drink?
- School calendars disrupted, facilities submerge as Lake Baringo waters rises again
- How Karimenu II Dam, new partnerships are reshaping water security
- New prawn project targets snails threatening health and harvests in Kenya
Keep Reading
The theme was chosen based on feedback from an online survey among stakeholders from the human, animal, plant, and environmental health sectors, which collected nearly 200 responses globally.
AMR is not only a pressing global health and socioeconomic crisis. It also has significant impacts on human and animal health, food production, and the environment. The World Bank estimates that AMR could result in US$ 1 trillion in additional healthcare costs by 2050 and US$ 1 trillion to US$ 3.4 trillion in gross domestic product (GDP) losses per year by 2030.
Dr Loice Ombajo, an infectious disease specialist at the University of Nairobi, says AMR is a global threat, but it is worse in low- and middle-income countries due to the financial burden it imposes on people living in these countries.
"If we are not able to treat them because they are resistant to the drugs, the cost of care becomes expensive, and people die. We are in a crisis, and we should begin to act now to curb AMR," she warns.
Dr Ombajo observes that the most common cases of AMR occur through the overuse and misuse of antibiotics, which many people buy over the counter.
"We must learn to use antibiotics properly. Don't buy antibiotics over the counter; they should only be prescribed by a qualified doctor. You should also finish your dose whenever you are on antibiotics and don't take leftover antibioticsm," she says.
Another cause of AMR is using antibiotics wrongly. According to Dr Ombajo, statistics show that many people use antibiotics to treat colds and flu, which are caused by viruses.
"Antibiotics kill bacteria and not viruses, so when you take antibiotics for a sore throat, you are making the bacteria in your body become resistant to drugs such that if you get sick and require antibiotics, it will be hard to treat them," she explains.
Dr Romona Ndanyi, the deputy director of veterinary services in the Ministry of Agriculture and Livestock, says drug-resistant-pathogens pose a threat to everyone, everywhere. Yet, much more can be done to raise public and stakeholder awareness.
She emphasizes that antibiotics must be used properly, even on animals, since many pathogens could easily end up on our dining tables. Dr Romona says there is a period you have to wait before you sell or consume the meat or milk from animals that have been treated with antimicrobials.
"Dairy farmers should wait for at least three days from the last day the antimicrobial has been given. Livestock and chicken farmers should stay at least 30 days before selling or consuming the meat," she advises.
Dr Romona explains that AMR that animals transmit can be prevented by training farmers on food husbandry and farm hygiene to ensure that animals are properly fed.
She advises that people should follow the appropriate Water, Sanitation, and Hygiene (WASH) procedures across all sectors to prevent infections.
"Even the water we give animals should be clean. We should also vaccinate our animals to prevent diseases. Everybody should take action and realise that it is a global health concern. Our political leadership should realize that they are also vulnerable to AMR," she says.
The 2022 Global Antimicrobial Resistance and Use Surveillance System (GLASS) report highlights alarming resistance rates among prevalent bacterial pathogens. Median reported rates in 76 countries of 42 per cent for third-generation cephalosporin-resistant E. coli and 35 per cent for methicillin-resistant Staphylococcus aureus are a major concern, for urinary tract infections caused by E. coli, 1 in 5 cases exhibited reduced susceptibility to standard antibiotics like ampicillin, co-trimoxazole, and fluoroquinolones in 2020. This is making it harder to treat common infections effectively.
"For us to be able to tackle AMR, we have to use the one health approach
One Health refers to an integrated, unifying approach that aims to achieve optimal and sustainable health outcomes for people, animals, and ecosystems," she says.
According to WHO, Tuberculosis (TB) is also a major contributor to antimicrobial resistance. Multidrug-resistant tuberculosis (MDR-TB) is a form of TB caused by bacteria that do not respond to isoniazid and rifampicin, the two most effective first-line TB drugs. Only about two in five people with drug-resistant TB accessed treatment in 2022.
Dr Romona says AMR is a complex problem that requires sector-specific actions in the human health, food production, animal, and environmental sectors and a coordinated approach across these sectors.
"One Health refers to an integrated, unifying approach that aims to achieve optimal and sustainable health outcomes for people, animals, and ecosystems. It recognizes that the health of humans, domestic and wild animals, plants, and the wider environment are closely linked and interdependent," she says.
The One Health approach to preventing and controlling AMR brings together stakeholders from relevant sectors to communicate and work together in the design, implementation, and monitoring of programs, policies, legislation, and research to mitigate AMR and attain better health and economic outcomes.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.