A new non-surgical heart procedure is proving to be a game changer, especially for patients with critical underlying conditions.
Traditionally, such patients were treated through open heart surgery, where the damaged heart valve was replaced with an artificial one. However, these surgeries, particularly for elderly patients or those with multiple comorbidities, carry significant risks and in some cases, can result in fatal outcomes.
To reduce exposure for patients with underlying heart issues, Nairobi West Hospital has introduced the Transcatheter Aortic Valve Implantation (TAVI) procedure. This minimally invasive procedure is designed to replace a narrowed aortic valve that fails to open properly.
This breakthrough marks a significant advancement in cardiac care, especially for high-risk patients who are not ideal candidates for conventional surgery.
According to Dr VijaySinh Patil, an Interventional Cardiologist at The Nairobi West hospital, the procedure takes just one hour and is performed while the patient is conscious.
"The procedure is unique for the aortic valve. Patients with a lot of calcium or blockage or leakage in the valve can undergo this procedure," says Dr Patil.
- Kenyan doctors perform rare heart procedure
- Silent threat: A sore throat could lead to rheumatic heart disease
- Doctors told me I would lose my life to rheumatic heart disease in 15 days
- Why men need more exercise than women to see the same heart benefits
Keep Reading
The patient who underwent the procedure had visited the hospital with complaints of breathing problems and fatigue and was advised to consider the procedure as a permanent solution.
"I came to The Nairobi West Hospital and, after a series of tests, decided to undergo the procedure after Dr Patil explained that I had a heart condition. I was initially a bit tense, but he assured me it was a non-invasive procedure that would take less than an hour. I had been suffering from the condition for a few years, and it had worsened over time. The doctors told me it would be life-threatening if not addressed," says Godfrey Mbithi, who is from Nyeri.
Dr. Patil explains that aortic stenosis, a condition where the aortic valve narrows and restricts blood flow from the heart, has traditionally required open-heart surgery to replace the damaged valve.
"The TAVI procedure involves placing a new valve within the diseased aortic valve through a catheter, usually inserted via the femoral artery in the groin. Using advanced imaging, the new valve is precisely positioned and expanded within the damaged valve, restoring proper blood flow. This minimally invasive approach results in shorter hospital stays, faster recovery, and fewer complications compared to traditional surgery," Dr Patil explains.
Recent advancements in TAVI technology have further improved its safety and efficacy, expanding its use to patients with intermediate and even low surgical risks. As the population ages and aortic stenosis becomes more prevalent, the demand for TAVI is expected to grow.
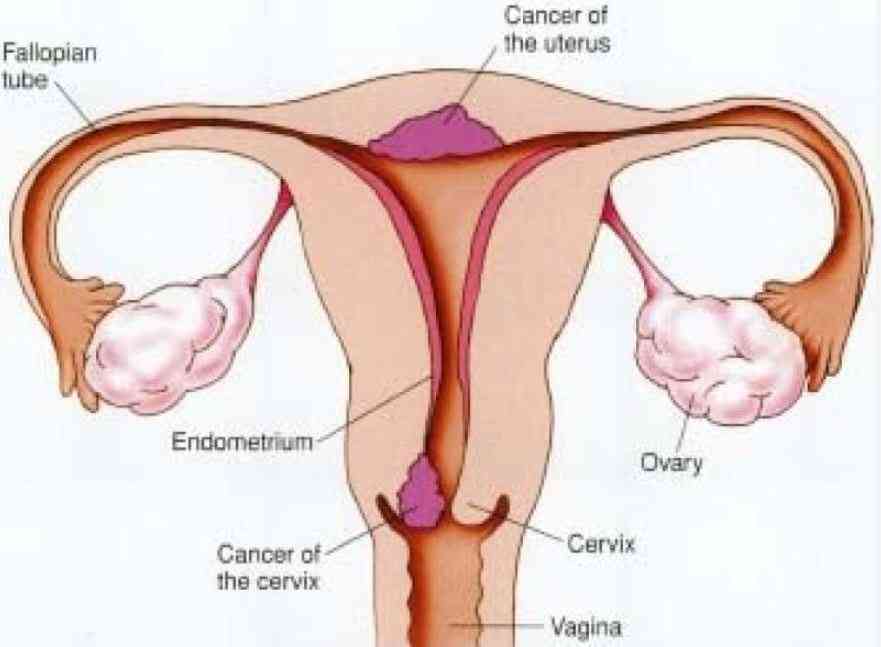
"This development comes as heart disease, once more common in developed countries, now spreads rapidly to developing nations like Kenya. For many of these countries, heart attacks strike like a sudden storm, catching governments unprepared as they focus resources on malaria, HIV/AIDS, and child mortality, often neglecting non-communicable diseases," observes Dr. Patil.
In 2020, the World Health Organization raised the alarm, noting that 60% of the global heart disease burden now lies in developing nations. Cardiovascular diseases claim 17.3 million lives each year and account for one in ten deaths in Africa. "Kenya lacks precise statistics on heart disease among its citizens, but in South Africa, someone suffers a heart attack or chest pain every seven minutes, totaling over 74,000 incidents annually," Dr Patil adds.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.