Tabitha Onyango is worried about the health of her newborn baby.
Born on March 25 at the Mlaleo Health Centre in Mombasa, the infant is yet to receive the polio jab that is out of stock countrywide.
At birth, the boy only received the Bacillus Calmette-Guerin (BCG) jab to protect against Tuberculosis, but polio vaccine was out of stock.
"I am worried about my baby's health. He is crying uncontrollably and is unable to stretch as he used to at birth," Onyango shares her fears, with tears in her eyes.
Onyango's search for vaccines mirrors the struggle facing mothers with newborns, who desperately want their children vaccinated against various deadly childhood diseases amid the biting vaccine shortage across the country.
Meanwhile, the Ministry of Health has acknowledged the shortage of vaccines namely BCG, measles, polio, rotavirus and tetanus.
Other out-of-stock vaccines include pneumococcal, human papillomavirus (HPV) and malaria, vaccines that were supplied by Gavi-the Vaccine Alliance.
The jabs are supplied through the Kenya Expanded Programme on Immunization (Kepi) which was established in 1980.
The shortage of vaccines, supplied and distributed by Gavi-the Vaccine Alliance and the United Nations Children's Fund (Unicef), is attributed to Kenya being qualified as a middle-income nation by the World Bank. This means Kenya has attained epidemic control and influence.
With the country's new economic status, international donors scaled down their input as the years progressed. But now, Kenyans are grappling as a crisis takes root.
Apart from immunisation, other heavily donor-funded programmes coming to an end include Tuberculosis (TB), family planning and HIV/AIDS.
Dr James Nyikal, member of the National Assembly Health Committee and one of the brains behind the Community Health Volunteers (CHV) programme, says Kenya is ill-prepared to sustain these health programmes.
"Kenya knew as early as 2003 that Gavi funding for childhood vaccines was to come to an end," he says.
"I remember there were plans on how to start putting more of our own money on vaccines, so that as time was getting by, our amount would increase so that by the time they (donors) are going, we are adequately funded. We do not do that. We just keep depending on them," he adds.
Dr Nyikal regrets that the failure of a transition plan risks the lives of more than 1.6 million children who are currently benefitting from the vaccination programme.
"Being made a middle-income country means we are now not entitled to some of this support, yet we have not planned our budget to take care of the gap," says Dr Nyikal, also a member of the Health Committee in the National Assembly.
"When you get to donor agreement on funding, many times you actually know in advance how long the fund is going to run, and therefore should start increasing your contribution to that project gradually so that you take over, particularly for a programme that will take a longer time," he says.
According to Allan Maleche, Executive Director of Kenya Legal and Ethical Issues Network on HIV and Aids, ending donor funding is likely to paralyse health services.
Kenya heavily depends on donor funding in the management of three killer diseases namely HIV and Aids, TB and Malaria, money which is funnelled through the Global Fund and U.S. President's Plan for AIDS Relief (Pepfar).
AIDS Healthcare Foundation Country Director, Dr Samuel Kinyanjui, notes that reducing funding for HIV, TB and malaria is likely to increase cases and mortalities.
"What we are seeing as stakeholders in health, especially in HIV and TB, is that the government is struggling to eliminate the diseases, and we doubt its capacity to meet the gap that will be left by donors," says Dr Kinyanjui.
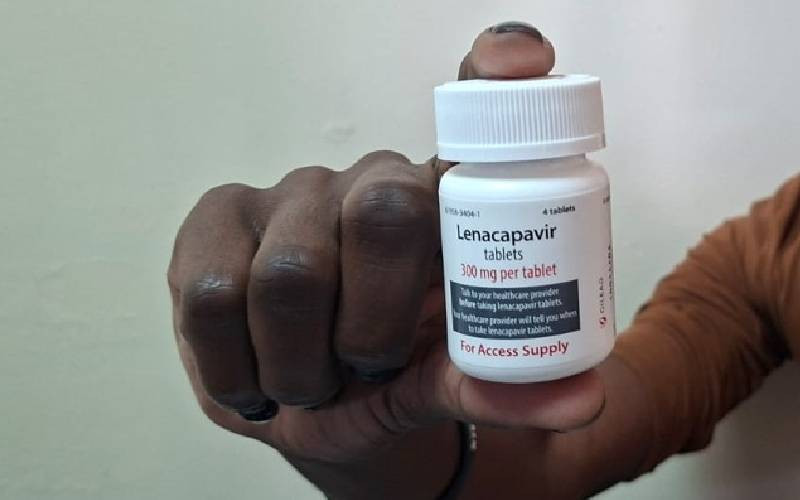
Kenyans have been accessing Antiretroviral (ARV) therapy and HIV services, thanks to Global Fund, which has been a game changer in fighting HIV. The funds also bridge the gap in the prevention of mother-to-child transmission.
Under this programme, donors supply commodities including testing kits and ARVs. At least 1,377,784 people are living with HIV/AIDS in Kenya, with plans to end HIV by 2027, as pronounced by President William Ruto.
However, Maleche says the government must invest in treatment, and care and remove the legal, social and policy barriers that affect people in treatment.
"It will be a difficult task for the government to achieve zero new infections by 2027 if they do not increase the funding to handle treatment, care and structural barriers," says Maleche.
Under 2024/25 budget estimates, HIV, family planning and vaccine commodities have not been funded by the National Treasury, despite the Ministry of Health requesting Sh14.1 billion for the same.
In the budget, the ministry had estimated counter funding to TB at Sh339 million and an additional Sh164 million for pending bills. Public Health PS Mary Muthoni pleaded with The National Treasury to consider picking up the funding for the programmes.
"There has been a steady reduction in donor funding for these programmes and therefore calls for the need to increase Government of Kenya counterpart funding to offset the deficit, especially for these medical commodities that are critically needed," the PS told the National Assembly Health Committee.
Kenya has also witnessed a shortage of family planning devices like free condoms in the recent past, resulting in unwanted pregnancies and sexually transmitted diseases.
The country receives family planning support from the Global Fund and the United Nations Population Fund (UNFPA). As donors zip up their wallets, Kenya is expected to step up to the challenge, but only time will tell.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.