In 2005, Nelima*, a young expectant mother, found herself in the maternity ward at Siaya Central Hospital. Unbeknownst to her, she carried a life-altering secret: she was HIV-positive. It wasn't until she was about to give birth that doctors informed her of her status.
"When the nurses found out I was HIV-positive, some refused to touch me," Nelima recalls. "They even stopped assisting me." Despite the stigma, her son was born HIV-negative. She attributes his survival to her prayers and her strict adherence to the little guidance she received from doctors.
"I knew very little about protecting my child from contracting HIV through breastfeeding," she says. "Back then, the stigma was immense. People believed that simply sharing a cup or touching someone with HIV could lead to infection. . It's by the grace of God that my son is now 19 and HIV-free."
While Nelima's story ended with hope, recent data reveals a troubling picture of mother-to-child HIV transmission (MTCT) trends in Kenya.
Despite earlier progress, challenges such as funding cuts, service disruptions, and shifting demographics threaten to reverse years of gains.
Dr Calvine Lwaka, Country Manager for the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF), highlights the critical issues.
"Many expectant mothers delay or skip antenatal care visits, missing opportunities for early detection," he says.
"Without timely HIV testing and treatment, the risk of transmission during pregnancy or breastfeeding increases."
- Oluga urges counties to prioritise HIV prevention amid rising youth infections
- Concern over rising HIV infections among the youth
- How drug abuse threatens fight to end Aids deaths, HIV infections
- Alarm over rising HIV rates among women in Bungoma
Keep Reading
According to the 2024 National Syndemic Disease Control Council (NSDCC) report, Kenya's MTCT rate stands at 7.3 per cent. However, counties like Kakamega (14 per cent), Busia (11 per cent), and Pokot (17 per cent) far exceed the national average.
Conversely, traditionally high-prevalence regions such as Siaya and Homa Bay have reduced rates to below 7 per cent, thanks to targeted interventions and community awareness programs.
Supply chain disruptions
The Covid-19 pandemic exacerbated existing vulnerabilities. Dr Lwaka explains how supply chain disruptions affected access to diagnostic tools and antiretroviral drugs.
"Delays in critical interventions for preventing transmission became more common," he says.
Additionally, demographic shifts have introduced HIV to previously low-risk areas, straining underprepared healthcare systems. Funding reductions have further limited the reach of prevention programs, especially in undeserved regions.
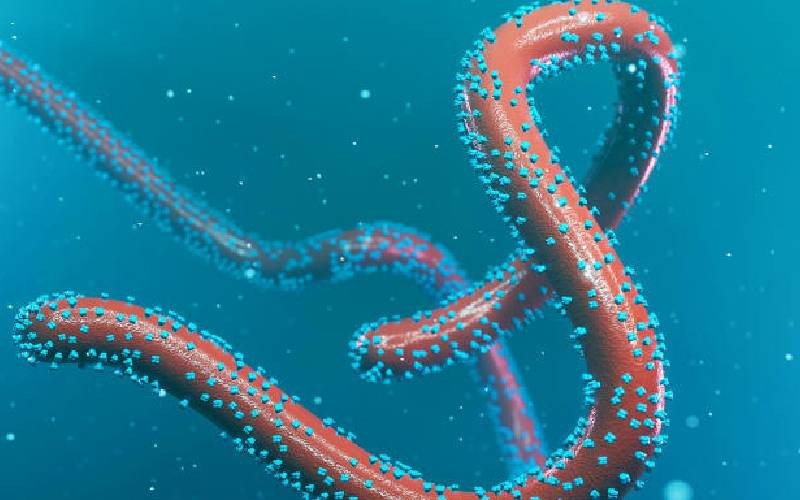
Globally, UNAIDS reports that nearly 150,000 children were newly infected with HIV in 2023-a 14 per cent increase from pre-pandemic levels. Sub-Saharan Africa remains disproportionately affected.
Dr Lwaka emphasizes that preventing MTCT requires a comprehensive strategy: Enhanced Antenatal Care (ANC), partner involvement and frequent viral load checks ensure adherence to anti-retroviral therapy (ART).
The doctor adds providing anti-retroviral medications to infants until breastfeeding cessation, followed by confirmatory HIV tests is very important.
When discussing ARVs for children, it's crucial to consider both treatment and preventive therapy. ARVs for children are formulated to suit their needs, often in liquid form or as dispersible tablets, as children generally face difficulties swallowing pills. Additionally, these medications may be flavored to improve acceptance.
In cases where a mother is HIV-positive, preventive measures,
"The mother must consistently take HIV treatment to maintain a low viral load, significantly reducing the risk of transmission during breastfeeding."
Regular testing
The child receives preventive ARVs during breastfeeding, typically using a combination of nevirapine, zidovudine, and lamivudine. This therapy continues for the breastfeeding period and an additional six weeks after cessation to ensure complete protection.
The doctor explains, regular testing is essential during this process, at 2-, 9- and 18-months antibody testing post-breastfeeding.
These steps help determine whether the child has contracted HIV. If the child tests positive, they are promptly started on lifelong treatment.
The key difference between ARVs for children and adults lies in formulation. Children's medications are designed to be palatable and easy to administer. Adults, on the other hand, typically take standard pills or tablets.
Like any medication, antiretrovirals (ARVs) can cause side effects, often most noticeable when treatment begins.
Barriers
While many diminish over time, severe adverse effects may require medication adjustments by healthcare providers.
Mothers and caregivers play a crucial role in observing changes in the child's health, reporting issues during clinic visits, and ensuring timely interventions.
Healthcare workers regularly assess children on ARVs, making adjustments as needed. Severe side effects are reported to national programmes for further review.
"If a child struggles with ARVs or breastfeeding risks increase, mothers may be advised to switch to alternative feeding options," explains Dr Calvine Lwaka.
Efforts to improve ARV administration include child-friendly liquid formulations, dispersible tablets, and flavouring. Kenya's "PAMA care" model integrates medical, psychological, and social support for families, streamlining care.
However, cultural taboos surrounding sexual health education remain a barrier. "Providing young people with knowledge about safe sexual practices is crucial," says Dr Lwaka, advocating for school curricula and community workshops to combat stigma and misinformation.
As Kenya tackles these challenges, technological innovation offers hope. Dr Charlie Maere, a global leader in digital health at EGPAF, highlights how artificial intelligence (AI) is revolutionising HIV care.
Over 400 Kenyan healthcare facilities now use AI-driven electronic medical record (EMR) systems to predict mother-to-child transmission risks or treatment defaults, enabling timely interventions.
"AI acts as a co-pilot for clinicians, providing actionable insights," says Dr Maere.
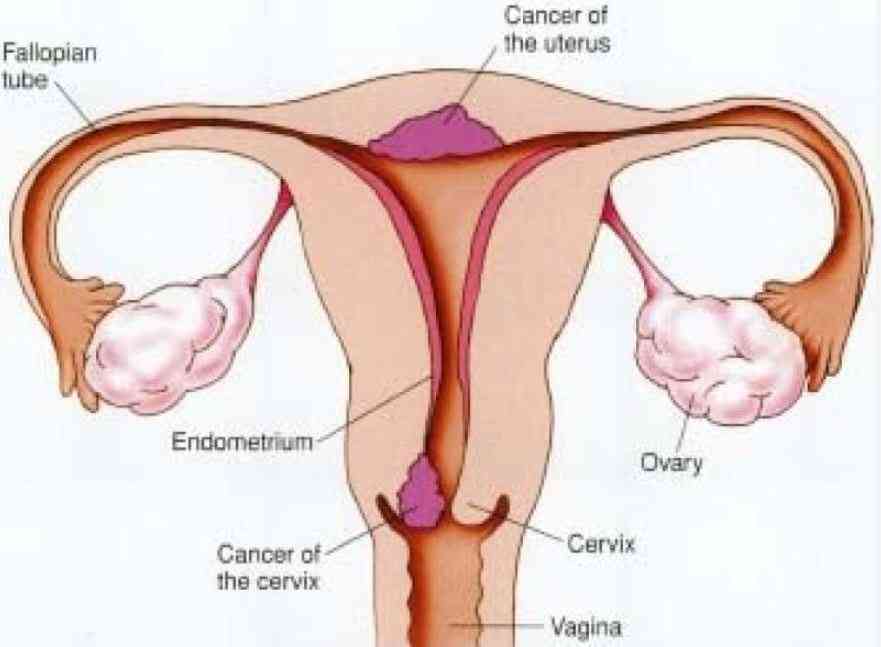
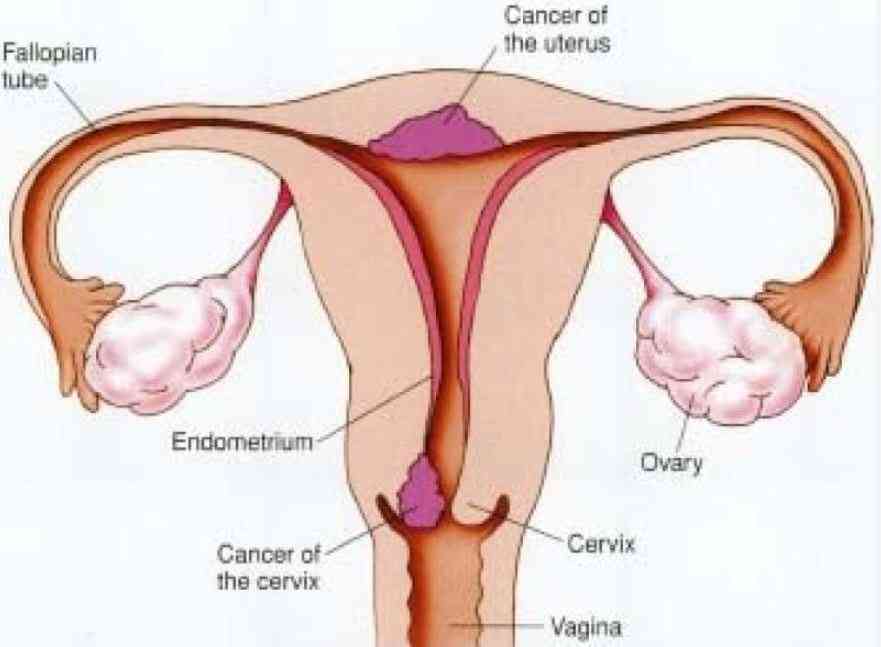
These systems flag high-risk cases, aiding proactive care, and are also used in diagnosing conditions like tuberculosis and cervical cancer in underserved regions.
Looking ahead, AI integration with national health records could allow patients to access personalised advice via mobile apps.
"HIV transmission is preventable," stresses Dr Lwaka. "It demands commitment from government, healthcare providers, and communities alike."
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.