Across many of Kenya’s counties, it is not uncommon to find women and young girls waist-deep in river water washing clothes or taking a bath.
It is a normal way of life for them as they remain ignorant of the fact that doing this exposes them to parasites that can cause irreparable damage to their uterus. These parasites, known as Schistosomes, are water-borne flatworms or blood flukes that enter the human body through the skin.
Once these flatworms are in the body, they develop into adult schistosomes and a person is then said to be suffering from Bilharzia or Schistosomiasis.
The adult worms live in the blood vessels where the females release eggs which are passed out of the body to continue the parasite’s life-cycle. Those that remain become trapped in body tissues, causing immune reactions and progressive damage to organs.
According to Centers for Disease Control and Prevention: “Freshwater becomes contaminated by these parasites’ eggs when infected people urinate or defecate in the water. The eggs hatch and if certain types of freshwater snails are present in the water, the parasites develop and multiply inside the snails. The parasite leaves the snail and enters the water where it can survive for about 48 hours”.

Neglected Tropical Diseases National Programme Director Dr Sultani Matendechero says the disease is one among 18 neglected tropical diseases.
He says the disease has very adverse effects yet continues to receive little emphasis in terms of awareness creation or steps being taken to control its spread.
Data from the World Health Organisation (WHO) shows that an estimated 258 million people required preventive treatment for schistosomiasis in 2014. Out of these, only 61.6 million were reported to have received treatment.
There are two major forms of schistosomiasis, intestinal and urogenital, and Dr Matendechero says what makes this illness especially detrimental to women is that these parasites affect their urogenital system and then moves on to the uterus.
“Once the disease strikes, it creates pockets of infections in the uterus that look like any other infection. Many health practitioners will assume the woman is suffering from a normal infection and will administer antibiotics,” he says.
Matendechero says the patient will not respond to this treatment regime and doctors will give them even stronger antibiotics, yet the infection will not clear.
“Antibiotics cannot clear bilharzia and as the disease continues to fester, the patient’s womb will develop sandy patches then the infection will start affecting blood vessels,” he says.
The next step after this is that the disease will start forming pus pockets in the uterus and then it will get very inflamed.
“Many times when the womb’s condition gets to this state, a misdiagnosis of cervical cancer is made yet cancer cells cannot be found,” he says.
Matendechero warns that at this stage, if quick steps are not taken to fight the parasites, the womb becomes irreparably damaged and the only solution is to have it removed.
“What this disease does to the uterus is very painful. Imagine when the uterus belongs to a teenage girl and she is rendered infertile over something that is easily preventable and treatable. We must create awareness and tackle this illness,” he says.
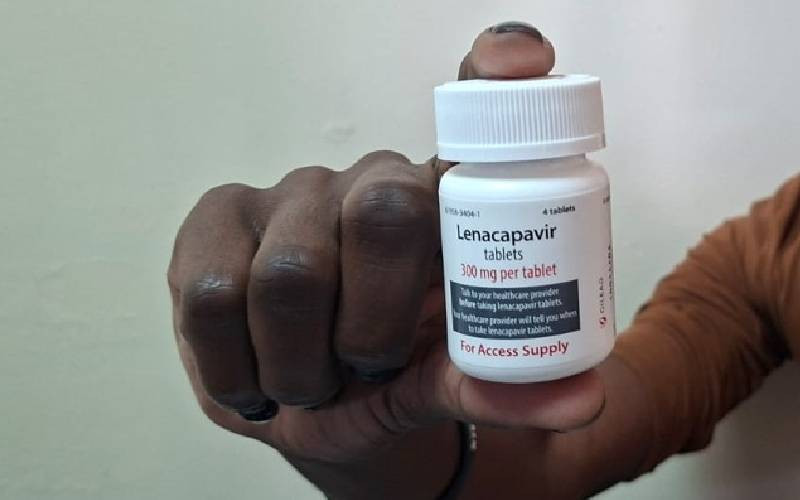
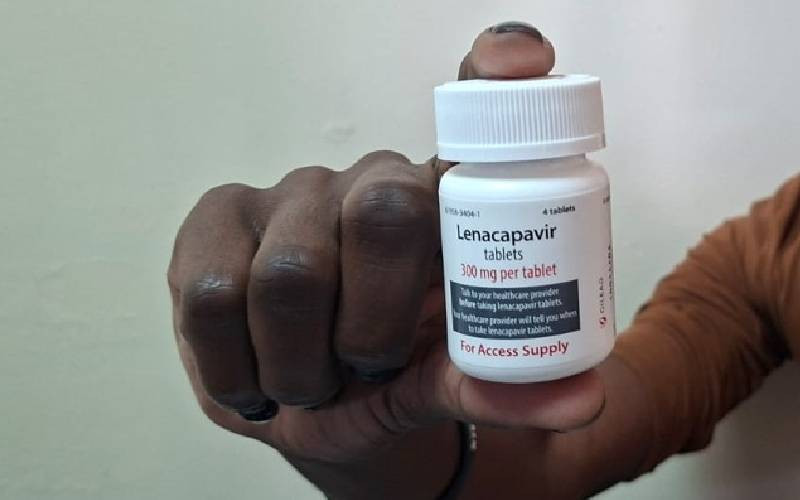
The doctor says the WHO recommended treatment for schistosomiasis is a tablet known as praziquantel, 40 miligrammes per kilogramme, taken as a single dose.
“Treatment can improve reproductive health of those affected and it is therefore advisable that young girls get regular treatment during mass drug administration,” he says.
Kenya Medical Research Institute (Kemri) Chief Research Officer, Dr Diana Karanja, says the organisation has already started conducting school based mass drug administration.
She saysthis follows results from a five year study on the prevalence of bilharzia along the Lake Victoria region conducted in 75 schools and 41 health care centres.
Releasing the results last week in Kisumu, Dr Karanja said the research carried out between March 2011 and May 2015 found existence of massive ignorance of the disease among medics in the region.
“Bilharzia is a disease that adversely affects cognitive development in children and should not be taken lightly yet its symptoms continue to be misdiagnosed as malaria,” she says.
Karanja says the other challenge is that health facilities do not have enough medicine to tackle the illness and those that do rarely administer them so the drugs end up expiring.
The Kemri team also identified the disease’s diagnostic process as a challenge since it is largely still being carried out through microscopy, although there are plans to introduce better user friendly kits.
“During the study period, test for the disease was done by taking stool samples from the children after parents consenting,” she adds.
Dr Karanja says her team decided to focus on the Lake Victoria region due to presence of the large fresh water body in an area where open defecation still happens.
“Only 38 of the 833 areas studied have been declared open defecation free zones. This means that sanitation and hygiene in these areas is still an issue, making it easy to transmit the disease,” she says adding that the study was carried out in three groups.
In the first group, pupils were treated every year for five years, the second lot were only treated for two years while the third batch received treatment for a year, skipped the next year and were treated again for a year.
At the end of this study period, Dr Karanja says they observed a considerable fall in bilharzia prevalence from 19 per cent to 8.5 per cent.
“The disease rate came down tremendously after the first treatment and it stabilised for the rest of the years,” she says.
The study also reveals that school absenteeism rates went down from four per cent in March 2011 to 1.5 per cent in May 2015. “Data from 2008 to 2011 indicated that absenteeism was high. But after beginning the study in 2011, absenteeism went down. We think this happened because the pupils got drugs to control the disease,” she says.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.