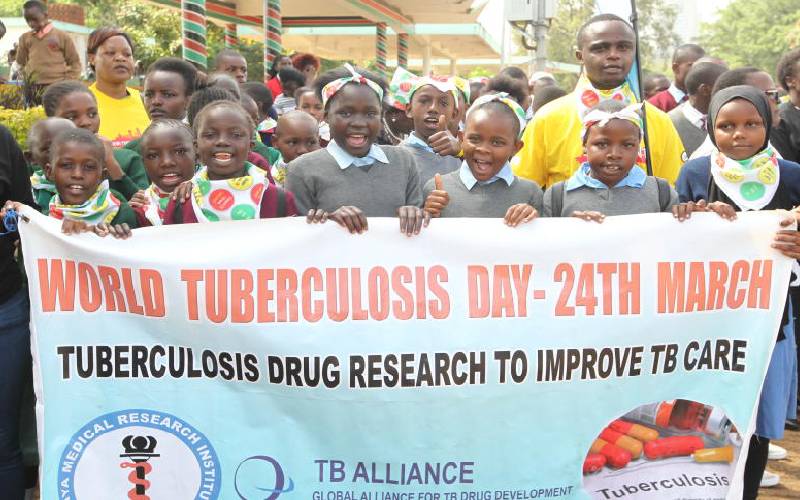
Pupils from schools in Nairobi take part in a two-kilometre walk that was among events meant to sensitise the public on the scourge of TB in our society. The World TB Day is being marked today. [Jonah Onyango, Standard]
In 2007, when the rest of the country was battling post-election violence, Apollo Ndirangu was battling Tuberculosis (TB).
It started as a normal cough that became persisted for two weeks. Then he started sweating at night and lost appetite.
He reluctantly decided to go to hospital in his Busia county. The doctors were clear with him; he had TB. Normally, Apollo was told, a mild form of TB can go away within six months if he sticks to the medication.
But given the stigma surrounding the disease, he stopped taking the drugs when he felt better before completing the full dosage.
Three months after stopping medication, the symptoms showed up again. He was directed by doctors to resume medication. Apollo again stopped taking the drugs when he got a job in Uganda.
Work requirements took him again from Uganda to Sudan, while ignoring his medication. He was not lucky. TB recurred and this time it attacked with sharper fangs than before. He was forced to come back home.
Doctors told him the disease had grown resistant to the drugs he was taking, and he would need a tighter treatment schedule that would last for two years.
The treatment involved receiving 240 injections that would go hand in hand with swallowing unimaginable number of pills; 13 in the morning and four in the evening.
It was on a Good Friday when trouble started. Apollo was supposed to receive his 153rd injection from a dispensary in his Mathayos village. He said in an interview that he went to the dispensary and found it locked.
Two more visits to the facility that Easter weekend were also not fruitful; it was locked.
He went the Tuesday after Easter and found doctors who accused him evading the injections. The doctors, he said, threatened him with jail time.
Apollo then ran away to Uganda. He was arrested there and hurled before Kenyan courts. He was sentenced to two years in prison while strict observation was made as he took the medicine.
He spent time at Korinda prison and was released in 2014. When he went home, his wife and child had left his house. Only his mother helped him with the healing process.
In Makueni county, the story of Muli Mulinge is the same. His life was prospering here in Nairobi when TB hit him.
His family took him home and sought help from Mukuyuni hospital where he was treated. The treatment regime was so dire that his family abandoned him.
A public health officer came to his rescue and linked him with one Kioko Mulatya, a community health volunteer in Makueni.
It was Mr Mulatya who helped him complete his treatment. Today, he lives alone near a hill in Nthongoni. He spends his days reminiscing sweet memories of the city.
According to the Public Health Act, isolation is a key preventive measure for control of infectious diseases.
Patients must be isolated until it is certified that they pose no danger to the community.
On March 24 2016, the High Court abolished imprisonment of TB patients who failed to take medicine.
It issued a directive to the Ministry of Health to develop an isolation policy where patients would be held in health facilities instead of prisons.
"If one poses a threat to the public, they can be isolated. The law allows isolation as the final measure," Allan Maleche, the Executive Director for Kenya Legal and Ethical Issues Network on HIV/AIDS said.
"Just like in Covid-19 cases, isolation should only be adopted during the period of infection."
Tuberculosis remains the fifth leading cause of death in Kenya. According to the Ministry of Health, at least 96,434 people were diagnosed with Tuberculosis in 2019.
Of these, 10,087 were children. Another 669 had been diagnosed with Multiple Drug Resistant Tuberculosis.
About 40 per cent of TB cases go without treatment annually. People aged between 15 and 44 years are the most infected with TB.
HIV patients are the most exposed to TB. Factors such as poverty and stigmatisation have led to an upsurge of TB in the country.
TB is a contagious airborne disease that spreads through the air. Due to this fact an isolation policy must be put in place.
The policy allows for two kinds of isolation - voluntary and involuntary.
Maleche argued that before TB patients are isolated, doctors should first understand the reasons why they are not taking their medicines.
"The patients could be suffering from side effects as a result of the TB drugs. Even as you trample on their right to liberty make sure you understand their medical needs," said Maleche.
In the last five years, Kenya has reported an annual decline in the number of reported TB cases at a rate of one per cent. Drug resistant TB continues to be a major public health challenge in Kenya.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.