×
The Standard e-Paper
Stay Informed, Even Offline
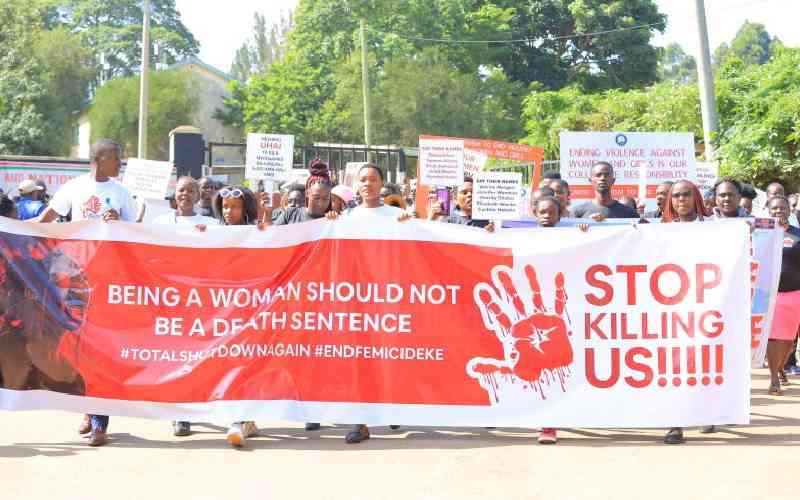
Each year, millions of women and children globally die from preventable causes.
Maternal, newborn and child health (MNCH) is a shared global priority, yet we often overlook one of its most pressing and preventable barriers: violence against women.