Did you know that for every ten babies born, one is preterm? And that every 40 seconds, one of those babies dies? This is according to a report released by United Nations Children’s Fund (Unicef), titled “Born Too Soon: A Decade of Action on Preterm Birth,” released in 2023.
Ashley Muteti, a mother of three girls, all born sooner than they were expected, knows fully well the challenges associated with giving birth to preterm babies. When she was expectant for the first time in 2017, Ashley’s pregnancy journey was smooth until the 24th week when she started feeling unwell.
“The doctor said I had severe pre-eclampsia. They put me on blood pressure medication, and then they tried to prolong the pregnancy to at least 30 weeks,” she narrates.
After delivering baby Zuri at 30 weeks, weighing 1.2 kilogrammes, Ashley and her husband had high hopes that their baby would survive, but this was not to be. “The journey was so draining because one minute, the baby was improving, and the next, she was not okay. Zuri developed complications, and her organs began failing. We were also told that she was bleeding in the brain,” she says.
Baby Zuri later succumbed to Necrotizing Enterocolitis while at the Newborn Intensive Care Unit (NICU).
Keep Reading
Shattered hopes
According to the Cleveland Clinic, Necrotizing enterocolitis (NEC) is a serious gastrointestinal problem that mostly affects premature babies. The condition inflames intestinal tissue, causing it to die. A hole may form in the baby’s intestines, causing bacteria to leak into the abdomen or bloodstream. NEC usually develops within two to six weeks after birth. In some infants, NEC is mild. Others experience severe, life-threatening symptoms.
“We were told that when and if she got to two kilogrammes, we would go home. She was so close to achieving this, and it was a difficult moment for us because we had done a lot of shopping for the baby and prepared so much for her.”
Dr Laura Oyiengo, a Maternal and Newborn Health specialist at Unicef Kenya, describes prematurity as babies who are born alive before 37 weeks of pregnancy are completed. She notes that prematurity is the leading cause of death in children under the age of five years.
As the World marked the International Prematurity Day on Sunday, November 17, it emerged that there is a need to raise awareness of preterm births and the concerns of preterm babies and their families.
“The Born Too Soon report shows that globally, 2.3 million children died in the first 20 days of life in 2022. There are approximately 6,500 newborn deaths every day, amounting to 47 per cent of all child deaths under the age of five years,” says Dr Oyiengo.
After losing her baby, Ashley had sworn never to get pregnant again. Six weeks after delivering baby Zuri, she was put on an Intra-Uterine Device (IUD) to prevent future pregnancies. However, just five months after they had buried baby Zuri, Ashley got pregnant. According to a report by Science Daily, women who give birth to a premature baby after developing pre-eclampsia are 17 times more likely to experience another preterm birth if pre-eclampsia emerges again.
“I remember being so devastated, and the doctor gave me two options … to either terminate the pregnancy or to keep the baby as a high-risk patient. Thanks to the support I got from my husband, we decided to keep the pregnancy,” she says.
Ashley continued to take high blood pressure medication. But at 24 weeks, she started feeling sick again. Her pregnancy was prolonged again up to the 30th week when she checked her blood pressure level, and it was too high. Ashley was rushed to hospital, and when the doctors did an ultrasound, they found out that the baby had stopped growing at 26 weeks. By the time she got to the hospital, Ashley was bleeding profusely, and both her life and the baby’s were in danger. They had to do an emergency delivery. Baby Amani was born weighing 975 grammes with breathing difficulties. She was resuscitated and immediately put in the NICU.
“Amani was so tiny, and this time, my husband and I decided not to spend a lot of energy and resources in the hospital because we did not see her surviving. We would go for only one hour, and we were out.”
Kangaroo care
On realising that the baby had a better chance of surviving, Ashley and her husband were told to come to the hospital more often and offer skin-to-skin care (Kangaroo care), which is essential for preterm babies. “The hospital ensured we had skin-to-skin interaction with the baby to help her gain weight, reduce the chances of infection, and regulate her heart rate. It also helped us bond with the baby,” she narrates.
Baby Amani stayed in the NICU for close to two weeks, after which she was taken to the Newborn High Dependency Unit. She had some breathing challenges and blood transfusions, which forced her to stay in hospital for three months. She is now five years old and healthy.
Dr. Oyiengo emphasises the need and importance of Kangaroo Mother Care. This cost-effective intervention can be practiced in a facility or at home and has been shown to improve the health outcomes of preterm babies.
“Unicef has collaborated with various county health ministries to establish Kangaroo Mother care units in health facilities and equip newborns to provide quality care to small and sick newborns. Unicef also supports the training of community health promoters on care for preterm babies and newborns discharged home from the hospital,” she says.
When Ashley thought she was done with giving birth, she got pregnant with an IUD again. This time, however, she was more aware and prepared for any eventualities. The year was 2020 when she gave birth to baby Nia at 35 weeks, weighing 2.3 kilogrammes. This was a great improvement from her previous deliveries. Ashley was delighted that she could sleep with her baby after delivery- for the first time.
“I enjoyed cuddling with baby Nia, unlike in the previous situations where my babies would be put on oxygen, numerous injections, and pipes. After three days, I went home with my baby.”
Although the experience with her third child was delightful, Ashley and her husband were too afraid to lose Nia that they would be so cautious and anxious.
“When you lose a child, death becomes so tangible that you are always afraid of simple things. We couldn’t believe that Nia was given a clean bill of health, so we kept checking and rechecking, even rushing to the hospital for minor things.”
Ashley adds that she was given medication for anxiety for fear of losing her babies. Besides that, she kept visitors away from her house for nine months.
“I would not want any mother and child to go through what I went through,” she says.
Creating awareness
This inspired her to come up with the Zuri Nzilani Foundation to help and support mothers with hypertensive disorders in pregnancies, infant loss, and premature births.
“Between 2023 and now, the foundation has supported more than 40 women to deliver their babies safely. We also do training, social support, advocacy, and research in a bid to ensure that every mother and child has the opportunity to thrive,” she says.
Symprose Okinda, a maternal health advocate, wife, and mother of two girls, also gave birth to her daughter before her expected delivery date.
“The baby was so tiny; I was shocked I could not comprehend many things because of anesthesia, but I remember wondering why my baby was brought to me in a polythene bag.”
Okinda, whose pregnancy journey was smooth until the third trimester when she was diagnosed with preeclampsia, emphasises the importance of attending antenatal clinics religiously.
“The moment you make up your mind to become pregnant, you should see a doctor so they can assess any risks that could be associated with your pregnancy. Start your clinics early. Many mothers start clinic at six months, making it hard for medics to prevent preeclampsia. Early detection and management can save lives,” says Okinda.
She appreciates that she had the support she needed when she gave birth to her baby, who weighed 1.3 kilogrammes at birth. However, Okinda will never forget the anxiety she experienced during the three months her baby was in hospital. She narrates how it was a rollercoaster of emotions throughout. Okinda’s daughter is now three years old and healthy.
Risk factors
Dr. Priscillah Koech, a neonatologist and lecturer at the University of Nairobi, explains the risk factors of giving birth to premature babies.
“Maternal factors include diseases in the mother, which could either be infectious or non-infectious. Diabetes and hypertension are also some of the risk factors because these conditions cause the environment in the womb to be hostile for the development of the baby.”
Dr Koech adds that mothers with incompetent cervixes may not be able to hold the baby to term.
Another risk factor, according to Dr Koech, is when the birth canal is closer to the urinary canal. This, she says, increases the risk of infections that could lead to preterm delivery.
“Younger mothers below 18 also face a higher risk of delivering prematurely since their reproductive systems are not usually fully developed,” she explains.
The challenge of inaccessibility to healthcare centres is also a risk factor, especially in rural areas where babies cannot access care.
“If the mother delivers away from the health facility, the baby will be exposed to cold and infections will follow. There needs to be an improvement in health facilities and health funding so that we have accessibility and well-equipped facilities,” she says.
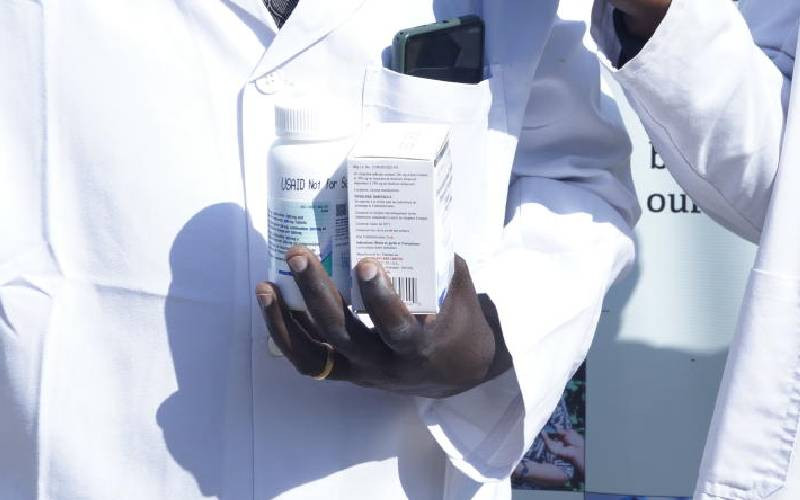
Unicef works with the Ministry of Health at the national and county levels and collaborates with other sectors (Health, WASH, nutrition, and climate adaptation) to ensure that preterm babies receive high-quality, comprehensive health promotion and preventive and treatment support.
At the National level – Unicef supports the development of strategies, policies, guidelines, and standards aimed at addressing the quality of care for preterm babies and other newborns.
“We support the development of national-level action plans, such as the Every Woman Every Newborn Everywhere (Ewene) action plan, which provides the roadmap for the country to scale up interventions that reduce preventable newborn mortality, including mortality among preterm babies,” says Dr. Oyiengo.