Reports of suspected mpox have sent the country on the edge, with the Ministry of Health dispatching health experts to Taita Taveta County, where the case was detected.
A truck driver was identified by Port health officers with a generalised rash at Taveta One Stop Border Point on July 22, 2024. The individual was reported having symptoms for two weeks prior.
The team, led by disease surveillance expert, Dr Pius Mutuku, pitched camp in the County to support the county health officials and also undertake contact tracing for those who might have come into contact with Patent Zero.
The government said it is undertaking all measures possible to ensure the disease does not spread.
Keep Reading
- No new mpox cases confirmed since July 22, Health ministry says
- Kenya confirms one Mpox case, steps up surveillance at border
- Africa Mpox resurgence fuels alarm
- WHO calls emergency committee on mpox spread
Health authorities say the patient had travelled through Uganda, Kenya, Tanzania and Rwanda and are working with neighbouring countries to identify any contacts and any other potential cases. There is an active Mpox outbreak in the Great Lakes Region, with DRC, Burundi, Rwanda and Uganda afflicted. However, the Central African Republic, which is currently in civil turmoil, is the worst affected, with the capital, Bangui, reeling in the wake of spiking cases.
Professor Julius Oyugi, a virologist and an expert from the University of Nairobi, says monkeypox is a viral disease just like Covid and HIV.
The first human case, he adds, was recorded in 1970 in central Africa in what is now referred to as DRC.
It is believed to have originated from Monkeys or rodents hence the name Monkeypox.
Because of the origin of monkeys, there are certain species of these apes, believed to be residing in the Tropical African forests, which are the main hosts.
The interaction between primates and humans is believed to have led to the virus' transmission from monkeys to humans.
Anyone arriving in Central and West Africa often suffers the culture shock of bushmeat. Big cities in DRC, including Goma, Lubumbashi and even Kinshasa, not forgetting Bangui, have flea markets where roast antelopes, monkeys, carpet pythons, tortoises, crocodiles and other reptiles are a big deal on the menus. The wildlife is hunted deep within the expansive Congolian forests, including the Congo, Ituri, and Ngaramba among others, where unhealthy interactions between the wildlife, some carriers of the viruses, happen.
Initially, Monkeypox was only concentrated in West and Central Africa. However, in 2021 the virus spread to other parts of the world including the U.S. mainly because of travel. Those infected passed the virus across the borders.
Symptoms
While most Kenyans are mgetting accustomed to the large, blister-like rashes, other symptoms of the disease include lesions, fever, intense headache, muscle aches, back pain, general body weakness and swollen lymph nodes, typically lasting two to four weeks. However, not every patient may display these symptoms.
But some mpox patients start showing signs of affliction between the first 4 and 11 days after infection. But in some cases a patient may start displaying these signs a day after being infected. Yet, around 5 percent of cases have been known to display symptoms after 21 days.
Unlike the virus that causes Covid-19, which spreads through tiny droplets expelled as one breaths, mpox is not as readily transmissible as it relies on close physical contact to transmit from one person to the other.
Currently, Kenya is on alert, as the East African Community calls for a heightened public awareness to combat the spread of the disease.
The World Health Organization (WHO) has since reported that Burundi, Central African |republic (CAR) and the Democratic Republic of Congo (DRC) are experiencing an outbreak of the viral Mpox disease.
Burundi has confirmed three (3) cases of Mpox in Bujumbura and Isare cities, verified by national laboratories and the WHO.
DRC has reported over 21,000 cases since 2022 and more than 1,000 deaths, according to WHO.
In 2023, there were 14,626 cases and 654 deaths, and by the end of May 2024, 7,851 cases and 384 deaths had been reported.
Burundi borders DRC, Rwanda and Tanzania, while the DRC, which is the second largest country in Africa by area after Algeria, borders five EAC Partner States: Tanzania, Burundi, Rwanda, Uganda and South Sudan.
EAC Secretariat, in a post on its website, says all partner States should educate their citizens on how to protect themselves and prevent the spread of Mpox.
EAC said it will convene a meeting of health experts to deliberate on the situation.
“However, in anticipation of pandemics and epidemics in the region, the EAC, with support from the German Government through its development arm GIZ and the Africa CDC, has established a pool of rapidly deployable experts ready to be sent to areas of disease outbreaks in the EAC,” stated EAC.
EAC said GIZ has also supported it in strengthening 10 border areas with the DRC and other EAC partner states by providing handwashing facilities and health promotion activities to encourage protective health and hygiene behaviours, aiming to prevent the spread of zoonotic and water-borne infectious diseases.
EAC Deputy Secretary General in charge of Infrastructure, Productive, Social and Political Sectors, Hon Andrea Aguer Ariik Malueth, in the post on their website emphasised the importance of taking preventive measures to minimise the spread of Mpox.
“EAC Partner States must provide necessary information about the disease and take preventive measures,” said Malueth.
According to Lancet Global Health, the struggles of Eastern African countries in managing the latest surge in mpox cases highlight the gaps that exist between the global north and south.
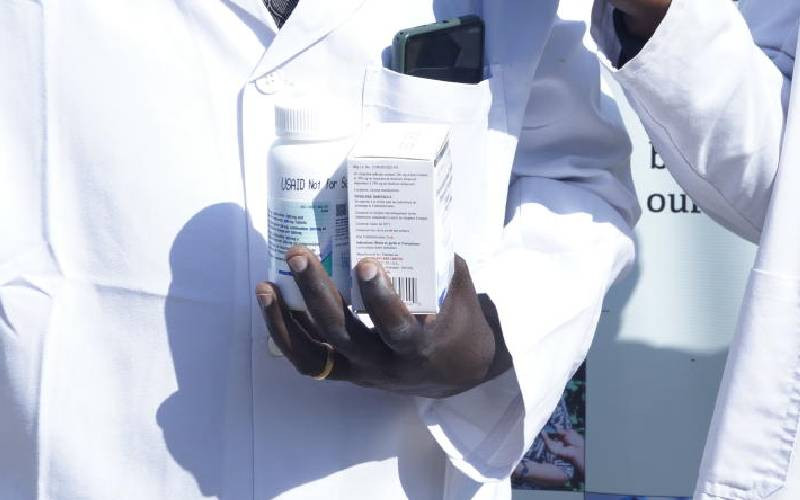
“The recent mpox outbreaks highlight global inequities in resource allocation and access to vaccines, diagnostics, and treatments. MpoxReC advocates for the rapid expansion of these medical countermeasures, with concurrent implementation studies to better characterise their distribution, safety, and effectiveness in African contexts,”, says a report shared on the organisation’s website.
The report also pushes for an African-led solution.
“We have proposed the establishment of an African-led, multidisciplinary, multicountry Mpox Research Consortium (MpoxReC) in Africa with an overarching goal of establishing a research network to advance the elimination of mpox as a public health problem (with an initial focus on Cameroon, the Central African Republic, the Democratic Republic of the Congo, Ghana, Nigeria, and the Republic of the Congo),” adds the report.
This evokes the dark memories of Covid-19 vaccine inequalities, where Western nations hogged and hoarded vaccines as the disease ravaged third-world countries amid a scramble for the few available jabs.
South Africa, on whose soil some vaccines were manufactured by the Aspen Pharmacare, could not have some of the products used locally due to the contractual obligations. With the latest outbreak of yet another possible viral contagion that could test Africa’s healthcare systems and response readiness, only time will tell, for mpox is not just another monkey’s affair, but a threat to humanity.