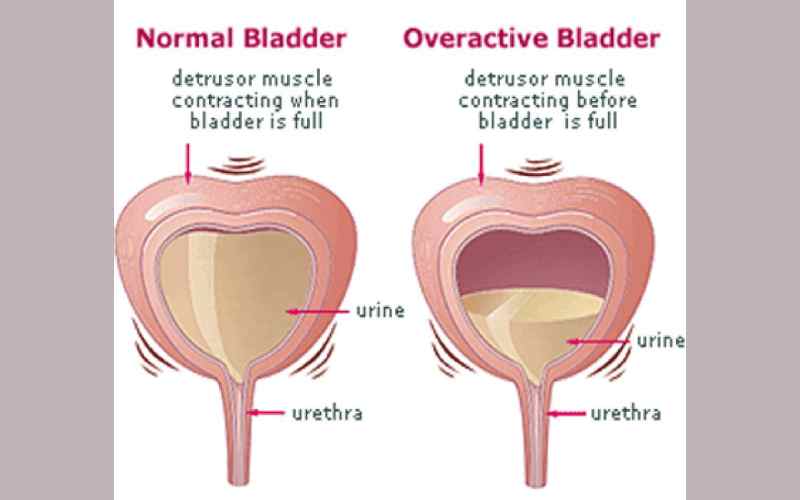
Overactive bladder describes a combination of chronic and bothersome urinary symptoms such as abrupt, uncontrolled urge to urinate, possible urine leaks and going to the bathroom many times during the day and night. Research published on PubMed estimates that nearly 17 per cent of the overall adult population experience OAB. The International Continence Society describes the urinary urgency as so strong to ignore. Majority of the patients who suffer from OAB are of advanced age. Most of the time, these patients show no sign of an obvious underlying issue such as urinary tract infection, urinary incontinence or metabolic disorders that affect urination.