The ongoing doctors' strike is set to enter its fourth week. That would mean a full month of total paralysis in public healthcare services. While this is not a new phenomenon in the country, the current healthcare workers' strike opens the lid on systemic failures that exist not only in the health sector but also across other sectors.
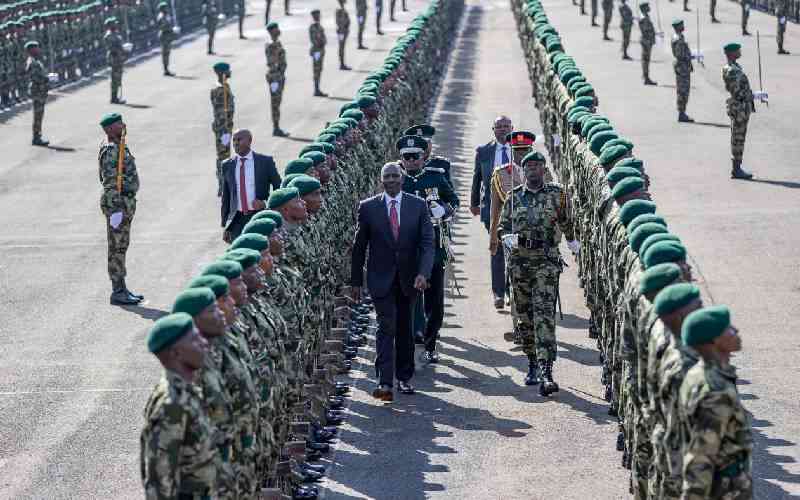
Ever since assuming office 19 months ago, the KK administration has demonstrated a unique penchant for more money through taxes and levies on anything and everything they can place their hands on.